Smart buildings need smart solutions for connected networks and building controls. A command center brings it all together.
And it's not just about technologically integrated "smart" buildings. Brendon Buckley, Healthcare Technology Director at Johnson Controls, stated at HealthSpaces (Almost) Live that there has long been a need for managing very complex operations centrally.
"I'm willing to bet that the first command center you ever saw was NASA's Mission Control," he said. "The amazing problem-solving skills and the brainpower combined with state-of-the-art technology and communications really made it seem like there was absolutely nothing that they couldn't accomplish or do."
But command centers aren't just for the advanced science of space travel; hospitals need them, too.
The Four Types of Hospital Command Centers
There are four basic types of command centers that hospitals use today, Buckley explained: incident response centers, security operations centers, facility or building operations centers, and capacity management or care progression centers.
Almost every hospital in America has some form of an incident response command center, and they are activated when they are needed in the case of emergencies, which may range from severe weather events to mass casualty events, and, as we've recently learned, pandemics. There are also internal incidents that can be security incidents or the occasional IT outage.
A security command center, or security operations center, performs surveillance as well as integrated services around threat detection and alarm management response. The security operations center is able to dispatch officers and staff to help manage any type of safety concern.
"That's really the benefit of having the security operations center," Buckley said. "It provides that centralized look and approach to managing the security of hospitals today."
Building operations centers are also important, especially given the complexity of the systems that it takes to operate a modern-day hospital. Building management, fire, medical gas, and even nurse call systems can be integrated into the facility command center. Buckley said that the building operations center is often where the operators are located so they can dispatch code blue alerts or other types of clinical emergency events. This center also includes the asset management system, which can include real-time location systems and automate guided vehicles to deliver medication, linens, and even meals to patients.
"Having that centralized visibility and control of these facilities systems within the hospital is absolutely critical," he said.
One of the biggest challenges for hospitals today is capacity management.
"Hospitals can have a huge impact and benefit if they are able to manage the patient throughput – benefits that impact safety, satisfaction, and operational efficiency – which really helps a hospital operate the best it can," Buckley said.
The capacity management command centers typically focus on bed management – making sure that beds are available for patients and that they’re not waiting if a bed is sitting unused, making sure environmental services is aware if an empty bed needs to be turned and the room cleaned, and making sure patients are being transported from the OR or ED. Capacity management also means making sure that when patients are ready to leave that they are able to do so in a quick and orderly fashion instead of having to wait around, thus tying up that bed, slowing down throughput, and reducing capacity.
The capacity command centers provide the information coming from all of these different systems, and also make sure that care is coordinated between the different teams that would handle bed management, environmental services, transport, and discharge. The command center approach really allows operators to take advantage of having those services in the same room and able to communicate with each other.
How the Command Center Needs to Evolve
Buckley believes there is a real opportunity to think beyond the silos of clinical systems and building systems, not just from a technology standpoint but also from a process standpoint. And nothing is better for integrating processes than a command center.
First, he'd like to see more integration of asset management into command centers, as there are elements of incident response tied into asset management as well as PPE and other assets that are so critical to the delivery of care.
He also believes that understanding the flow of patients is absolutely necessary, both inside and outside of the hospital.
"I think understanding and being able to take care of those patients outside the four walls of the hospital is absolutely important, so I think the command center has to have telemedicine capabilities incorporated," he said.
Additionally – and this is very much a lesson learned from the pandemic – they need to be able to operate virtually and decentralized. "People can get sick and pandemics can spread very quickly. You can have this amazing command center but nobody can physically be there, so being able to operate that in a decentralized approach virtually absolutely needs to be considered."
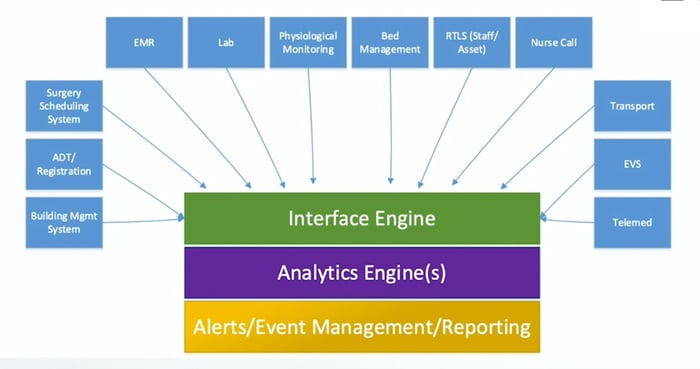
Also leveraging data sources from outside of the organization – third party sources, affiliates, and partners – is incredibly important because that data can really be beneficial to hospitals, especially as they start looking more at predictive analytics. Additionally, being able to normalize data – display it, act on it, and generate alerts and reports based on it – is crucial for improving hospital operations and driving better outcomes.
Common Mistakes to Avoid
As beneficial as command centers are, they aren't foolproof. There are some typical mistakes Buckley sees hospitals make in how they design and deploy their command centers, and the most frequent one is "noise."
"It's really easy to get excited about the technology and to do the technology for technology's sake, and let's be honest: the NASA command centers look really cool," he said. "But you've got to be careful of that. That 'noise' I'm referring to can be a visual distraction; it doesn't have to be audible.
Having huge displays and tons of monitors and all the bells and whistles … well, that's a lot of bells and whistles. People can get alert fatigue, which can potentially be dangerous (in addition to simply being exhausting).
"Be weary of how much technology you put in, and make sure you understand the value and the benefit so that you're only using and displaying what you absolutely have to in that command center," Buckley advised.
 |
He also sees a problem with decision bottlenecks.
"We think that if command and control is centralized, it must be good. That is false," he said. "You really need to understand what decisions need to be made out in the field as opposed to a command center given the speed of response and the situational awareness."
He said that hub-and-spoke models can make sense for those types of command centers, but again warns against automatically assuming that everything has to come through the command center in order to be important.
Buckley also cautioned against trying to address everything at once. "It's just not possible. You're going to have to be okay with just picking three or four of your top areas that you need to address to make that command center successful," he said.
Then phase in the rest over time. "It's okay to wait a year or two. We're seeing that as a best practice now. We're still seeing that occasional command center where they were very ambitious, and unfortunately they really struggle during deployment and in making it a success."
How to Get There
The first thing Buckley recommends is to create a multi-department stakeholder steering committee.
"This is the team that is really focused on what the goal is of that command center," he said. He recommends planning and visioning workshops with diverse representation that includes multiple different departments, and not just the usual suspects. Different departments with different needs and different perspectives can identify processes that need to be fixed and issues that need to be addressed. Those "outside" groups are able to bring awareness to issues that others might not have even considered.
The next thing that needs to be done is identifying key pain points and making sure they are prioritized. How are these things measured? What does "good" look like?
"You want to get a number of goals and metrics that you're trying to impact narrowed down up front as much as you can," Buckley said. "Identify the challenges. Take them head-on. What is going to keep your organization from being successful in delivering in this command center and really realizing the value of it?" Knowing, as they say, is half the battle.
Buckley also recommends developing use cases and building them out with diverse teams, including representation from IT, clinical, and facilities, to get everybody on the same page as to what that vision is and what it means for them and their specific departments.
Last but not least, Buckley said don't be afraid to break it all up into phases.
"Rome wasn't built in a day. Nor will your command center be."

Posted by
Collaborate with your Peers!
HealthSpaces is a community for people that plan, design, build and operate spaces where healthcare is delivered.
June 7-9, 2026 | Braselton, GA
Learn More




-4.png)
-Dec-09-2025-05-48-44-4379-PM.png)
-4.png)
-1.png)
-2.png)

Comments